
Prof Mason
Liverpool Foot and Ankle Clinic
To book an appointment, either email or phone the number below or click the link.
E-mail: CVDWclerical@outlook.com
Contact Patient Liaison: 07717580737
Freiberg's Disease (Freiberg's infarction)

What is Freibergs Disease?
Freiberg’s disease is a rare condition affecting the metatarsal head (the rounded end of the long bone just before the toe), most commonly the second toe joint. It occurs when the bone and cartilage at the joint surface become damaged, leading to pain, stiffness, and difficulty walking.
It is sometimes described as a form of osteochondrosis or avascular necrosis, meaning the bone temporarily loses its normal blood supply and strength, resulting in the possible collapse of the bone.
Who usually gets Freiberg's disease?
The condition can affect any individual, occurring in approximately 1 in 2,800 people. However, there are some populations that its more frequent. An these are:
- Most common in adolescents and young adults
- More frequent in females
- Usually affects one foot
- The second toe joint is affected in the majority of cases
How does it occur?
The exact cause is not fully understood, but Freiberg’s disease is thought to develop due to a combination of factors, including:
- Repetitive overload of the metatarsal head
- A long second metatarsal, which takes more weight during walking
- Altered forefoot mechanics, such as a hypermobile first ray
- Reduced blood supply to the metatarsal head
- Metabolic or medical factors (e.g. diabetes, cholesterol disorders)
- Occasionally, a genetic or congenital predisposition
Importantly, it is not usually caused by a single injury, but by repeated stress over time
What are the symptoms?
Pain
- Pain is typically felt in the ball of the foot, most commonly under the second toe, but not always
- Pain is usually worse when walking, standing, running, or pushing off
- Early on, pain may settle with rest, but later it can become more persistent
- Some patients describe a deep, aching pain, while others notice sharp pain with activity
Swelling and tenderness
- Swelling around the affected toe joint is common
- The joint may feel tender when pressed
- Shoes may feel tight or uncomfortable over the ball of the foot
Stiffness and reduced movement
- The toe may feel stiff, particularly first thing in the morning or after rest
- Reduced ability to bend or straighten the toe
- As the condition progresses, movement at the joint may become increasingly limited
Walking and activity limitation
- Pain with prolonged walking or standing
- Difficulty participating in sports or physical activity
- A tendency to shift weight away from the painful toe, which can cause discomfort elsewhere in the foot
Mechanical symptoms
- Some patients notice a feeling of catching, grinding, or clicking in the toe joint
- A sensation that the joint is “not moving smoothly”
- In later stages, the joint may feel unstable or deformed

Changes in the toe or forefoot
- The affected toe may appear swollen or slightly misaligned
- Callus formation under the ball of the foot due to altered weight-bearing
- Over time, the joint can become enlarged or arthritic in appearance
Progression of symptoms
- Early stages may cause intermittent pain only with activity
- Moderate stages often lead to daily pain and stiffness
- Advanced stages can result in chronic pain, arthritis, and reduced toe function, even during normal daily activities
Important points
- Symptoms often worsen gradually rather than starting suddenly
- Pain is typically activity-related and centred on a single toe joint
- Early recognition and treatment can help slow progression and improve outcomes
How is Freiberg's disease diagnosed?
Freiberg’s disease is diagnosed by combining your symptoms, physical examination, and imaging tests. Early diagnosis is important, as treatment options and outcomes are better in the earlier stages of the condition.
X-rays
Plain X-rays are the most important initial investigation.
They can show:
- Flattening or collapse of the metatarsal head
- Irregularity or fragmentation of the joint surface
- Narrowing of the joint space
- Arthritic changes in more advanced disease
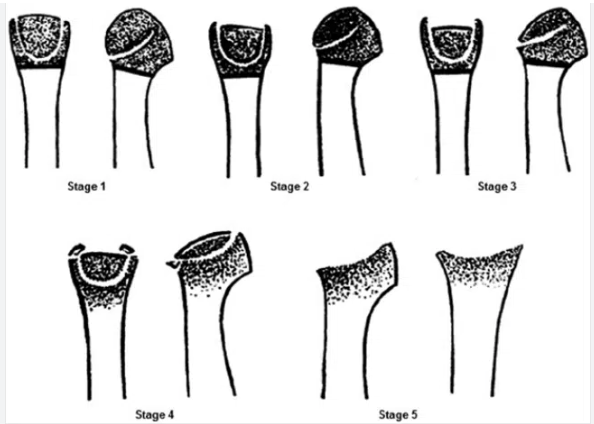
X-ray findings are often used to classify the condition into Smillie stages (I–V), which help guide treatment decisions.
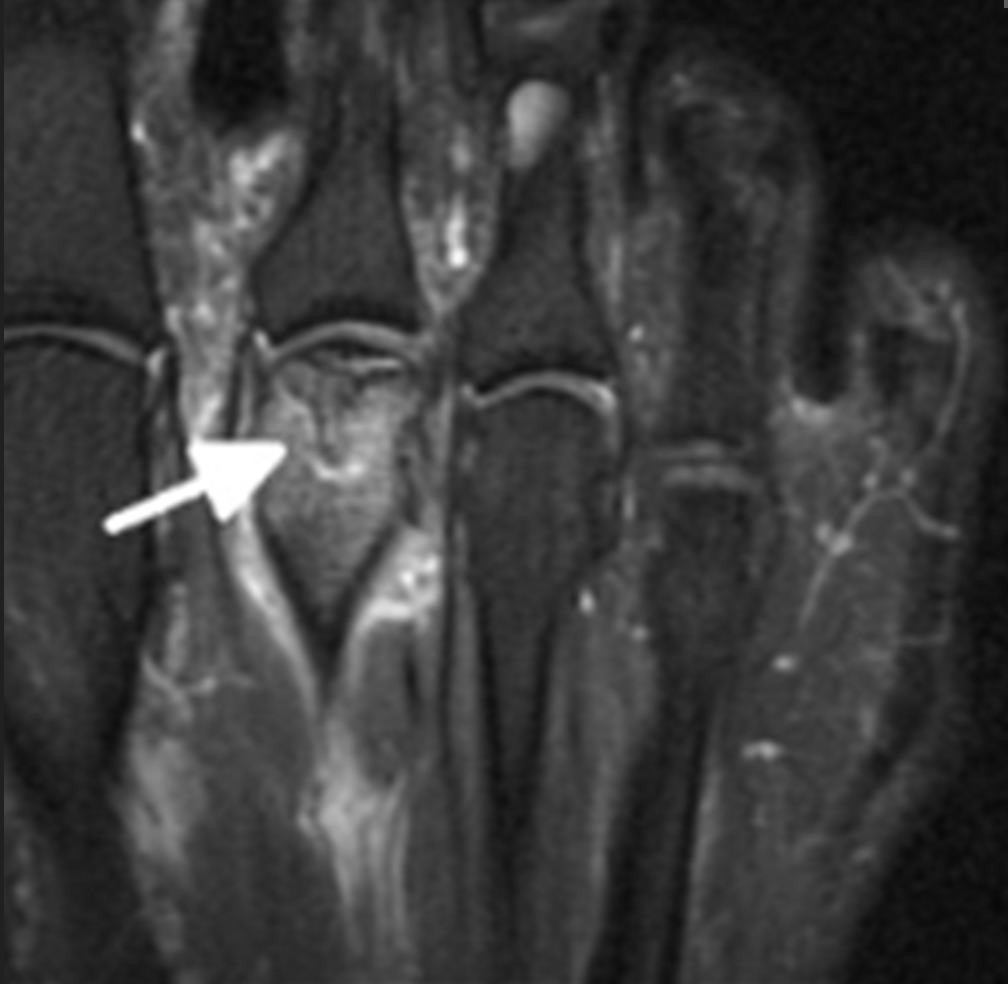
MRI scan
An MRI scan may be used when:
- Symptoms are present but X-rays appear normal
- Early-stage disease is suspected
- There is uncertainty about the diagnosis
- Surgical planning is required
MRI can detect:
- Early bone changes before collapse occurs
- Bone marrow oedema
- Cartilage damage
- The extent of joint involvement
This makes MRI particularly useful in early Freiberg’s disease.
X-ray findings are often used to classify the condition into Smillie stages (I–V), which help guide treatment decisions.
MRI is good at showing active and latent disease, especially in the early stages where X-rays are sometimes not useful
Non-surgical treatment
Non-surgical treatment is usually recommended for early stages of Freiberg’s disease (Smillie stages I–II) and for patients whose symptoms are mild or intermittent. The aim is to reduce pain, off-load the affected joint, and slow disease progression while the bone and cartilage attempt to recover.
Activity modification
Reducing activities that overload the ball of the foot is essential. This may include limiting running, jumping, prolonged standing, or high-impact sport. Complete rest is rarely necessary, but avoiding painful activities helps prevent further joint damage and allows symptoms to settle.
Footwear modification
Supportive footwear plays a key role in symptom control. Shoes with:
- A cushioned sole
- A stiff or rocker-bottom sole
- Adequate width in the forefoot
help reduce pressure through the affected metatarsal head. Thin-soled or flexible shoes tend to worsen symptoms and are best avoided.
Insoles and off-loading
Custom or prefabricated insoles can reduce load on the painful joint. These often include:
- Metatarsal pads or bars to shift pressure away from the affected toe
- Forefoot off-loading to reduce peak pressure during walking
Many patients notice meaningful pain relief with appropriate off-loading, particularly in the earlier stages.
Pain relief
Simple pain relief such as paracetamol or anti-inflammatory medication may help control symptoms, especially during flare-ups. These medications do not treat the underlying problem but can improve comfort while other measures take effect.
Physiotherapy
Physiotherapy focuses on:
- Improving foot and ankle mechanics
- Addressing calf tightness and forefoot loading patterns
- Gait advice to reduce pressure through the affected joint
While physiotherapy cannot reverse joint damage, it can help reduce symptoms and prevent compensatory problems elsewhere in the foot.
Immobilisation (selected cases)
In more painful early cases, a short period of reduced weight-bearing or use of a protective boot may be recommended. This is usually temporary and reserved for significant pain or flare-ups.
Expected outcomes
- Many patients with early-stage Freiberg’s disease improve with non-surgical treatment
- Symptoms may settle gradually over months rather than weeks
- Non-surgical treatment is less effective in advanced stages where joint collapse has occurred
Important points
- Non-surgical treatment aims to control symptoms and slow progression, not restore damaged cartilage
- Early diagnosis improves the chance of success
- Ongoing pain despite appropriate non-surgical care may lead to discussion of surgical options
Surgical Treatments
A wide range of operations have been described. The most commonly used and best-studied procedures are joint-preserving surgeries.
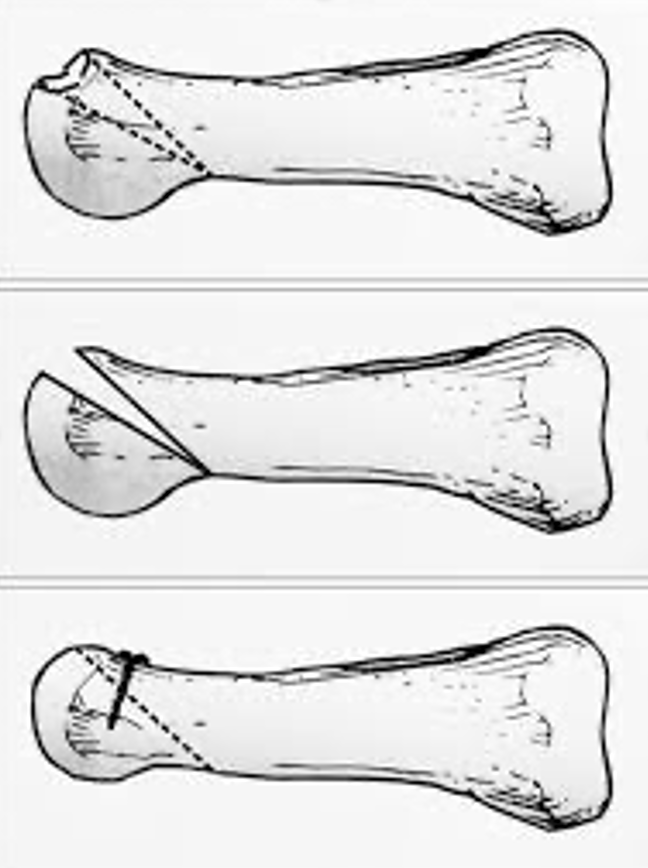
Dorsal closing wedge metatarsal osteotomy (DCWMO)
- A small wedge of bone is removed from the metatarsal
- This rotates healthier cartilage into the weight-bearing area
- Long-established technique with good pain relief
- Slightly shortens the metatarsal, which can affect foot mechanics in some patients
Autologous osteochondral transplantation
- A small plug of healthy cartilage and bone is taken from another joint (usually the knee)
- It is transferred to the damaged area of the metatarsal head
- Restores the joint surface without shortening the bone
- Associated with better movement, faster return to activity, and fewer complications in comparative studies
- Donor site problems are possible

Other procedures may be used in selected cases, including:
- Modified Weil osteotomies
- Microfracture or cartilage stimulation techniques
- Joint resurfacing or interpositional procedures (less common)
Recovery after surgery
- Usually protected weight-bearing in a boot initially
- Gradual return to normal shoes
- Physiotherapy to restore movement and strength
- Full recovery may take several months
- Most patients experience significant pain relief and improved function

