
Prof Mason
Liverpool Foot and Ankle Clinic
To book an appointment, either email or phone the number below or click the link.
E-mail: CVDWclerical@outlook.com
Contact Patient Liaison: 07717580737
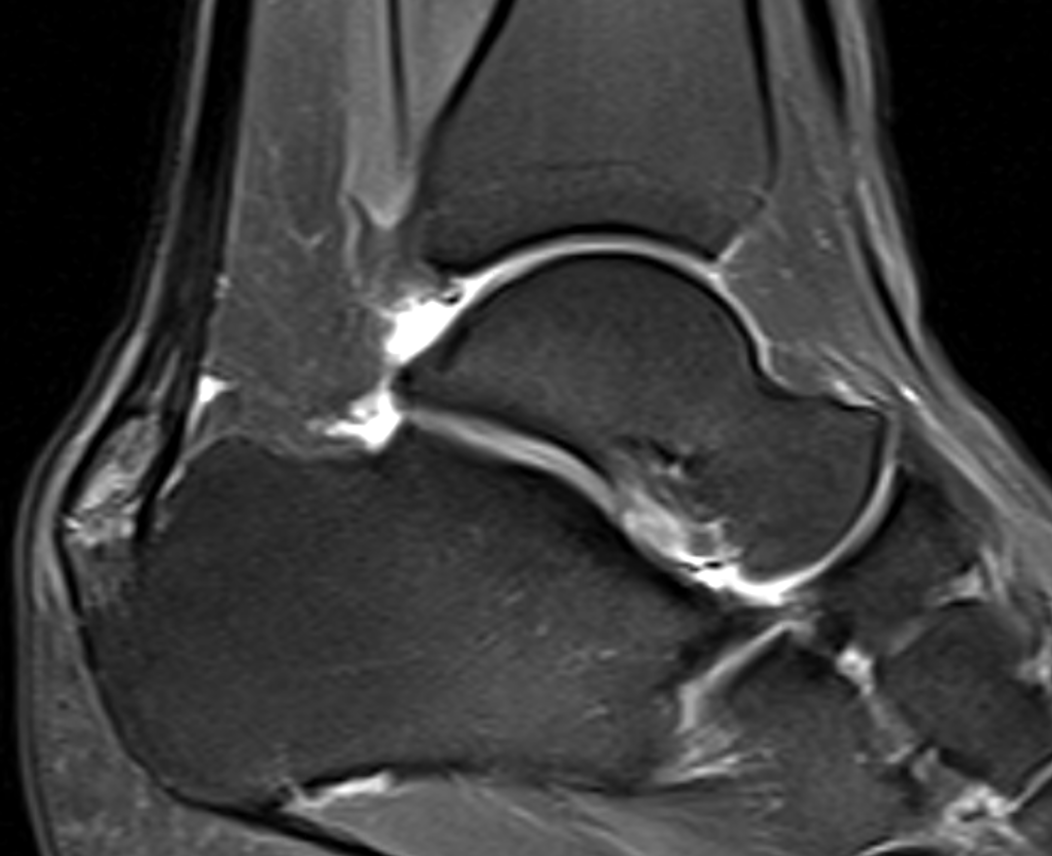
Heel Pain - Achilles Tendinopathy

What is Achilles Tendinopathy?
Achilles tendinopathy is a condition where the Achilles tendon (the strong tendon connecting your calf muscles to your heel bone) becomes painful and weakened due to repeated overload and reduced healing capacity.
It is not usually due to inflammation, but to changes within the tendon structure over time.
What are the types of Achilles Tendinopathy?
Non insertional (mid-portion) Achilles Tendinopathy
- Pain is felt 2–6 cm above the heel bone
- More common in active people
- Tendon may feel thickened or stiff
- Pain often improves with gentle activity, then worsens later
Insertional Achilles Tendinopathy
- Pain is located where the tendon inserts into the heel bone
- Often associated with pressure from footwear or a bony prominence
- Pain may be worse walking uphill, on stairs, or after rest
- Stretching into deep ankle movement can aggravate symptoms
The Causes Achilles Tendinopathy
Achilles tendinopathy develops when the tendon is loaded more than it can recover from. This usually happens gradually and is caused by a combination of mechanical strain, muscle tightness, activity patterns, and reduced tissue healing capacity.
1. Tight calf muscles (gastrocnemius and soleus tightness)
Tight calf muscles are one of the most important contributors to Achilles tendinopathy. When the calf is tight, the Achilles tendon is placed under increased tension with every step, particularly during walking uphill, climbing stairs, or running. Reduced ankle flexibility increases repetitive strain on the tendon and limits its ability to recover between activities.
2. Sudden change or increase in activity
A rapid increase in walking, running, sport, or exercise intensity is a common trigger. This includes returning to activity after a break, changing training surfaces, or increasing distance or speed too quickly. The tendon struggles to adapt when loading increases faster than its ability to strengthen.
3. Repetitive loading and insufficient recovery
The Achilles tendon experiences very high forces during normal activities such as walking and running. Repeated loading without adequate rest leads to microscopic tendon damage, which can progress to pain and tendon degeneration if recovery time is insufficient.
4. Footwear and mechanical irritation
Unsupportive footwear or shoes that rub against the back of the heel can aggravate the tendon, particularly in insertional Achilles tendinopathy. Flat shoes, worn-out trainers, or rigid heel counters can increase compression and irritation at the tendon insertion.
5. Body weight and load
Higher body weight increases the force transmitted through the Achilles tendon with each step. Even small increases in load, repeated thousands of times per day, can significantly increase tendon strain and contribute to symptoms.
6. Metabolic and medical factors
Conditions that affect tissue quality and healing increase the risk of Achilles tendinopathy:
- Diabetes
- Raised cholesterol or lipid disorders
- Reduced circulation
- Use of certain medications (including some cholesterol-lowering drugs)
These factors weaken tendon structure and slow recovery.

7. Age-related changes
As we age, tendons naturally become less elastic and have a reduced ability to repair themselves. This makes the Achilles tendon more vulnerable to overload and injury, even with activities that were previously well tolerated.
8. Work and lifestyle factors
Jobs involving prolonged standing, walking, or manual work increase repetitive loading through the tendon. A “weekend warrior” pattern—low activity during the week followed by intense activity at weekends—also places the tendon at higher risk.
9. Biomechanics and movement patterns
Poor movement control, altered walking or running mechanics, and weakness elsewhere in the lower limb can increase load on the Achilles tendon. These factors are often subtle and are addressed during physiotherapy.
Typical history and symptoms
Achilles tendinopathy usually develops gradually, rather than after a single injury. Patients often describe a slow onset of symptoms that worsen over time if the underlying causes are not addressed.
Pain location
- Non-insertional (mid-portion) Achilles tendinopathy: pain is usually felt 2–6 cm above the heel bone, often with local thickening or tenderness of the tendon.
- Insertional Achilles tendinopathy: pain is felt at the back of the heel, where the tendon attaches to the heel bone, and may be associated with swelling or irritation from footwear.
Pain pattern
- Pain and stiffness are commonly worse first thing in the morning or after periods of rest.
- Symptoms often improve after a short period of walking or warming up.
- Pain may then worsen again later in the day or after prolonged activity.
Activity-related symptoms
- Pain during or after walking, running, climbing stairs, or walking uphill
- Difficulty returning to sport or exercise
- Reduced tolerance for standing or walking for long periods
- Symptoms may fluctuate, with “good days and bad days”
Stiffness and weakness
- A feeling of stiffness or tightness in the calf and Achilles tendon
- Reduced push-off strength when walking
- Some patients notice reduced power or endurance in the affected leg
Swelling or thickening
- The tendon may appear thickened or swollen
- Tenderness when pressing on the tendon
- In insertional disease, redness or irritation at the back of the heel can occur due to shoe pressure
Non-surgical treatment
First-line treatment (most important)
Most patients improve with non-surgical treatment, but recovery can take several months.
Activity modification
- Reduce aggravating activities rather than stopping completely
- Avoid sudden spikes in exercise
Exercise-based rehabilitation
- Eccentric or progressive loading exercises are the most supported treatment
- Exercises are tailored to whether the problem is insertional or mid-portion
- Consistency over time is key
Calf flexibility and strength
- Improving calf muscle function reduces strain on the tendon
- Stretching is used carefully, especially for insertional disease
Footwear adjustments
- Supportive shoes
- Temporary heel raises may reduce tendon strain
- Avoid shoes that rub on the back of the heel (especially for insertional pain)
Second-line treatment
These treatments may be considered when symptoms continue despite several months of structured exercise rehabilitation, footwear modification, and activity adjustment. They are additions to, not replacements for, ongoing loading and strengthening programmes.
Shockwave therapy (ESWT)
Shockwave therapy uses controlled sound waves applied through the skin to stimulate healing within the Achilles tendon. It works by improving blood flow and encouraging tissue repair rather than providing immediate pain relief. Symptoms often improve gradually over several weeks to months. Shockwave therapy has good evidence as a second-line treatment for both insertional and non-insertional Achilles tendinopathy and is commonly combined with an exercise programme.


Injection treatments (PRP and high-volume injections)
PRP (platelet-rich plasma) injections use a concentration of your own blood to deliver growth factors to the tendon in an attempt to promote healing. High-volume injections aim to reduce pain by altering nerve sensitivity and reducing abnormal blood vessel growth around the tendon. Results vary between individuals, and improvement is usually slow rather than immediate, often developing over several months. These treatments may help some patients but are not universally effective.
Steroid injections
Steroid injections are generally avoided in the Achilles tendon because they can weaken tendon tissue and increase the risk of rupture. In rare, carefully selected cases, a steroid injection may be considered around the tendon (not into it) for severe pain, but this is uncommon, and can be associated with high volume injection. Steroids do not improve long-term outcomes and are not a routine treatment for Achilles tendinopathy.
Surgical Treatments
Surgery is uncommon and is only considered when symptoms have persisted for at least 6–12 months despite a well-structured programme of non-surgical treatment.
The aim of surgery is to reduce pain, remove damaged tissue, and correct factors that continue to overload the tendon, particularly calf tightness.
Recovery after surgery is gradual and requires commitment to rehabilitation.


Surgery for non-insertional (mid-portion) Achilles tendinopathy
What problems is surgery addressing?
In mid-portion Achilles tendinopathy, surgery targets areas of degenerative tendon tissue, thickening, scarring, and poor tendon gliding that prevent normal healing.
Common surgical procedures
- Debridement of damaged tendon tissue - diseased portions of the tendon are carefully removed, allowing healthier tissue to recover and remodel.
- Release of surrounding tight tissue (paratenon release) - this improves tendon movement and reduces pain related to scarring.
- Longitudinal tenotomies or minimally invasive techniques - small controlled cuts stimulate healing within the tendon.
- Gastrocnemius (calf) lengthening - performed when calf tightness is a major contributing factor. This reduces ongoing strain on the Achilles tendon and is associated with good functional outcomes.
In selected cases, endoscopic or minimally invasive techniques may be used, which can reduce wound complications and speed early recovery.
Expected outcomes
- Most patients experience significant pain improvement
- Return to daily activities and work is common
- Return to sport may take several months
- Recovery is gradual rather than immediate
What problems is surgery addressing?
Insertional Achilles tendinopathy involves pain where the tendon attaches to the heel bone and may include:
- Degenerative tendon tissue
- Bony prominence or heel spur
- Compression of the tendon against the heel bone
Common surgical procedures
- Removal of damaged tendon tissue
- Excision of bony prominence or heel spur
- Partial detachment and re-attachment of the Achilles tendon, when necessary, using strong anchors
- Gastrocnemius lengthening to reduce tendon strain and improve outcomes
- Zadeks procedure - taking a wedge out of the heel bone to take the prominence away from the Achilles tendon
Surgery may be performed using open or endoscopic techniques, with endoscopic approaches generally associated with fewer wound problems and faster early recovery in suitable patients.
Expected outcomes
- Most patients report good pain relief and functional improvement
- Recovery is slower than mid-portion surgery due to tendon re-attachment if performed
- Swelling and stiffness can persist for several months

